Bacterial Pustule: What You Need to Know
Have you ever noticed a small, pus-filled bump on your skin that just doesn’t seem like a regular pimple? It’s unsettling, I know. You might be worried about what it is, how you got it, and most importantly, how to get rid of it. I’ve been there myself, and it can be quite concerning. That little bump could be a bacterial pustule, a common skin infection that, while usually not serious, can be uncomfortable and even spread if left untreated. But don’t worry, because in this comprehensive guide, I’ll share crucial information about bacterial pustules—from identifying their causes and symptoms to effective treatment and prevention strategies. My goal is to equip you with the knowledge you need to manage these skin issues effectively.
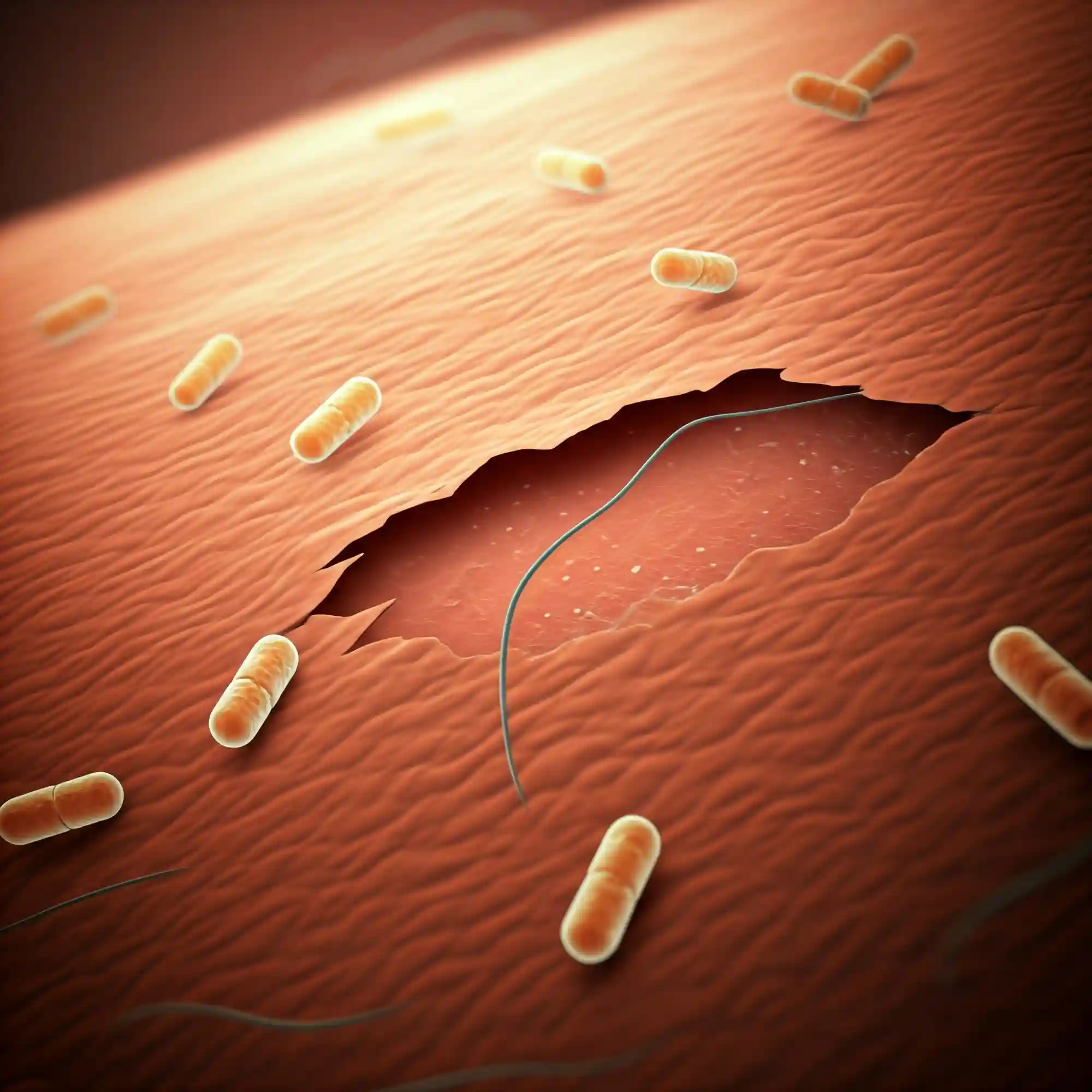
A bacterial pustule is a small, raised lesion on the skin filled with pus. This pus is a thick fluid containing dead white blood cells, bacteria, and cellular debris—a byproduct of your body’s immune system fighting off an infection. These pustules form when bacteria, most commonly Staphylococcus aureus (staph) or Streptococcus pyogenes (strep), enter the skin through a break, such as a cut, scrape, or insect bite. As your body’s immune system responds to this invasion, it sends white blood cells to the area to combat the bacteria. This process leads to inflammation and the formation of the characteristic pus-filled bump.
Bacterial pustules can appear virtually anywhere on your body, but I’ve noticed they frequently pop up on the face, neck, chest, back, and buttocks—areas where there are more hair follicles and sweat glands. While they are often harmless, understanding what they are, what causes them, and how to treat them is essential for preventing complications and promoting healing. In the following sections, I will delve into the details of bacterial pustules, providing you with the information you need to take control of your skin health. I want you to feel empowered to recognize, manage, and prevent these common skin issues.
Bacterial Pustule Causes and Risk Factors
From my experience, understanding the causes and risk factors of bacterial pustules is crucial for effective prevention and management. It’s like knowing what conditions encourage weeds in your garden—it helps you take proactive steps to keep them at bay. Several types of bacteria can lead to the development of these pustules, but the most common culprits are Staphylococcus aureus (often referred to as staph) and Streptococcus pyogenes (strep).
Staphylococcus aureus is a type of bacteria commonly found on the skin and in the nose of healthy individuals. While often harmless, it can cause a range of infections when it enters the body through a break in the skin. These infections can vary in severity, from minor skin issues like pustules and boils to more serious conditions like bloodstream infections and pneumonia. Methicillin-resistant Staphylococcus aureus (MRSA) is a strain of staph that has developed resistance to many common antibiotics, making it more difficult to treat. This is why proper hygiene and prompt treatment of skin infections are so important.
Streptococcus pyogenes, on the other hand, is known for causing a variety of infections, including strep throat, scarlet fever, and skin infections like impetigo and cellulitis. When it causes skin infections, it can also lead to the formation of pustules.
Now, let’s talk about the factors that can increase your risk of developing bacterial pustules. I’ve noticed that certain conditions and habits can make you more susceptible:
- Breaks in the skin: Cuts, scrapes, insect bites, and even dry, cracked skin can provide an entry point for bacteria. This is why proper wound care is essential.
- Weakened immune system: If your immune system is compromised due to illness (like diabetes or HIV), medication (such as corticosteroids), or age, your body is less able to fight off infections.
- Poor hygiene: Not washing your hands regularly, especially after touching potentially contaminated surfaces, can increase your risk of bacterial infections.
- Contact with contaminated surfaces or individuals: Sharing personal items like towels, razors, or sports equipment can spread bacteria.
- Certain medical conditions: Conditions like eczema or dermatitis can disrupt the skin’s natural barrier, making it more prone to infection.
Understanding these causes and risk factors can empower you to take proactive steps to protect your skin. Just like you would take measures to prevent pests and diseases in your garden, you can take steps to prevent bacterial pustules from taking root on your skin.
Bacterial Pustule Symptoms and Identification
Identifying a bacterial pustule correctly is the first step toward effective treatment. In my years of gardening and dealing with various plant ailments, I’ve learned that accurate identification is key to applying the right solution. Similarly, recognizing the specific characteristics of a bacterial pustule can help you differentiate it from other skin conditions and take appropriate action.
Here are some typical features I’ve observed:
- Appearance: Bacterial pustules are typically small, raised bumps on the skin. They have a characteristic white or yellowish center filled with pus, surrounded by a reddish, inflamed area. This redness is a sign of your body’s immune response to the infection.
- Location: While they can appear anywhere on the body, I’ve noticed they commonly occur in areas with hair follicles and sweat glands, such as the face, neck, chest, back, and buttocks. This is because bacteria can easily enter the skin through these openings.
- Associated Symptoms: Besides the visual appearance, bacterial pustules can also cause discomfort. You might experience pain, tenderness to the touch, and sometimes even itching in the affected area.
It’s important to differentiate bacterial pustules from other skin conditions, as the treatment approaches can vary. Here’s a quick comparison:
| Condition | Characteristics |
| Bacterial Pustule | Pus-filled, red, and inflamed; may be painful or tender. |
| Pimple (Acne) | Can be whiteheads, blackheads, or red bumps; typically not as inflamed as pustules and often associated with oil production. |
| Boil | Larger, more painful, and deeper than pustules; often starts as a red, tender bump and fills with pus over time. |
| Blister | Fluid-filled (clear, not pus); caused by friction, burns, or other trauma. |
If you’re unsure whether you have a bacterial pustule or another skin condition, it’s always best to consult a doctor or dermatologist for proper diagnosis and treatment. Just like I would consult an expert about a rare plant disease, seeking professional medical advice ensures you’re on the right track to recovery.
Bacterial Pustule Treatment Options
When it comes to treating bacterial pustules, I’ve learned that a combination of careful home care and, in some cases, professional medical intervention is the most effective approach. Just as different plants require different types of care, bacterial pustules may require varying levels of treatment depending on their severity.
For minor pustules, I often recommend starting with home care. These methods can often be enough to resolve the issue without the need for stronger treatments. Here are some key steps you can take:
- Warm Compresses: Applying a warm compress to the affected area for 15-20 minutes several times a day can help promote drainage and reduce inflammation. This is similar to providing consistent moisture to seedlings in your garden.
- Proper Hygiene: Gently cleansing the area with mild soap and warm water is crucial. Avoid harsh scrubbing, which can irritate the skin and potentially spread the infection. Think of it as gently weeding around delicate plants.
- Avoid Picking or Squeezing: I know it can be tempting, but resist the urge to pick or squeeze the pustule. This can worsen the infection and lead to scarring. It’s like trying to remove a weed by pulling on its leaves—you might break it off, but the roots will remain.
In some cases, over-the-counter (OTC) treatments can be helpful. Topical antibiotics, such as those containing bacitracin or neomycin, can help kill bacteria and promote healing. However, it’s important to use these products as directed and to consult a doctor if the pustule doesn’t improve within a few days.
Now, there are times when seeking professional medical attention is essential. I advise you to see a doctor if you experience any of the following:
- Signs of Spreading Infection: Increased redness, swelling, warmth, or red streaks extending from the pustule can indicate that the infection is spreading.
- Large, Painful, or Persistent Pustules: If the pustule is large, extremely painful, or doesn’t improve with home care after a few days, it’s time to see a doctor.
- Pustules Near Sensitive Areas: Pustules located near the eyes, nose, or genitals require medical attention due to the risk of complications.
- Signs of MRSA Infection: If you suspect a MRSA infection (which can be resistant to many common antibiotics), it’s crucial to seek immediate medical care.
Medical treatments for bacterial pustules can include prescription antibiotics (either oral or intravenous) and, in some cases, drainage of large abscesses. Your doctor will determine the best course of action based on the severity of your infection.
Bacterial Pustule Prevention, Control, Management, Care, and Protection
Just like I diligently protect my garden from pests and diseases, I believe in taking proactive steps to prevent bacterial pustules. Prevention, control, management, care, and protection are all intertwined when it comes to maintaining healthy skin. Here are some key strategies I recommend:
- Hygiene Practices:
- Regular Handwashing: Washing your hands frequently with soap and warm water, especially after touching potentially contaminated surfaces, is crucial. This simple act can significantly reduce the spread of bacteria.
- Keeping Wounds Clean and Covered: Any cuts, scrapes, or breaks in the skin should be cleaned thoroughly with mild soap and water and covered with a clean bandage. This creates a barrier against bacteria.
- Avoiding Sharing Personal Items: Sharing personal items like towels, razors, clothing, or sports equipment can easily spread bacteria. It’s best to avoid sharing these items whenever possible.
- Skincare:
- Gentle Cleansing: Use a mild, non-irritating cleanser to wash your skin. Avoid harsh scrubbing, which can damage the skin’s protective barrier.
- Moisturizing: Keeping your skin moisturized can prevent dryness and cracking, which can create entry points for bacteria.
- Lifestyle Factors:
- Maintaining a Healthy Immune System: A strong immune system is your body’s best defense against infection. Eating a balanced diet, getting regular exercise, and getting enough sleep can all help boost your immunity.
- Managing Underlying Medical Conditions: If you have any underlying medical conditions, such as diabetes or eczema, it’s important to manage them effectively, as these conditions can increase your risk of skin infections.
- Environmental Considerations:
- Cleanliness of Surroundings: Maintaining a clean environment, especially in areas where you spend a lot of time, can help reduce the presence of bacteria.
- Avoiding Contaminated Environments: If possible, avoid spending time in environments that are known to be contaminated with bacteria.
By incorporating these prevention, control, management, care, and protection strategies into your daily routine, you can significantly reduce your risk of developing bacterial pustules and maintain healthy, vibrant skin.
Complications of Untreated Bacterial Pustules
Just as neglecting a small problem in the garden can lead to a much larger infestation, ignoring a bacterial pustule can result in several complications. From my experience, prompt attention and proper care are essential to prevent these issues. While most bacterial pustules are relatively harmless and resolve with simple home care or over-the-counter treatments, neglecting them can lead to more serious health concerns. I want you to understand the potential risks so you can take appropriate action.
Here are some complications that can arise from untreated bacterial pustules:
- Spread of Infection: One of the most common complications is the spread of the infection to other areas of the body. This can happen if you touch or scratch the pustule and then touch other parts of your skin. It’s like transferring weed seeds from one part of your garden to another. The infection can also spread deeper into the skin, leading to more extensive skin infections.
- Formation of Larger Abscesses or Boils: If the infection is not controlled, it can progress to form larger, more painful collections of pus known as abscesses or boils. These are deeper infections that often require medical drainage.
- Cellulitis: This is a bacterial infection of the deeper layers of the skin and underlying tissue. It can cause redness, swelling, pain, and warmth in the affected area. In some cases, cellulitis can become quite serious and require antibiotic treatment.
- Sepsis: In rare but severe cases, a bacterial skin infection can spread to the bloodstream, leading to sepsis. This is a life-threatening condition that requires immediate medical attention. Symptoms of sepsis can include fever, chills, rapid heartbeat, and confusion.
- Scarring: Picking or squeezing pustules can damage the skin and lead to scarring. This is similar to how improper pruning can leave permanent marks on a plant. It’s best to avoid manipulating the pustule and allow it to heal naturally.
Here’s a table summarizing the potential complications:
| Complication | Description |
| Spread of Infection | Bacteria spread to other areas of the skin or deeper tissues. |
| Abscess/Boil | Larger, more painful collection of pus. |
| Cellulitis | Infection of the deeper layers of skin and tissue, causing redness, swelling, and pain. |
| Sepsis | Life-threatening bloodstream infection. |
| Scarring | Permanent marks on the skin due to damage from picking or squeezing. |
It’s important to remember that these complications are more likely to occur if the pustule is left untreated or if you have a weakened immune system. If you have any concerns about a bacterial pustule, it’s always best to consult with a healthcare professional. They can provide a proper diagnosis and recommend the most appropriate treatment plan to prevent any potential complications.
Bacterial Pustule FAQs
I often receive many questions about bacterial pustules, and I believe addressing these frequently asked questions will be beneficial for you. Just as I anticipate common questions about plant care and gardening techniques, I understand you likely have specific concerns about these skin issues. Here are some of the most common questions I encounter, along with comprehensive answers:
What are the best home remedies for bacterial pustules?
For minor bacterial pustules, several home care methods can be effective. Applying warm compresses to the affected area for 15-20 minutes several times a day can help promote drainage and reduce inflammation. Gentle cleansing with mild soap and warm water is also crucial, but avoid harsh scrubbing. It’s also essential to resist the urge to pick or squeeze the pustule, as this can worsen the infection and lead to scarring.
How to identify a bacterial pustule versus a pimple?
While both bacterial pustules and pimples are bumps on the skin, there are key differences. Bacterial pustules are typically filled with pus, have a white or yellowish center, and are surrounded by redness and inflammation. Pimples, on the other hand, can be whiteheads, blackheads, or red bumps and are often associated with excess oil production. Pustules are usually more inflamed and tender than typical pimples.
What causes bacterial pustules on the face and how to treat them?
Facial pustules can be caused by the same bacteria that cause pustules elsewhere on the body, such as Staphylococcus aureus. Factors like touching your face frequently, using contaminated makeup brushes, or having oily skin can increase the risk. Treatment for facial pustules is similar to treatment for pustules on other parts of the body: warm compresses, gentle cleansing, and topical antibiotics if necessary. However, it’s crucial to be extra gentle with facial skin and avoid harsh products that can cause irritation.
Are bacterial pustules contagious and how can I prevent spreading them?
Yes, bacterial pustules can be contagious, as the bacteria within the pus can spread to other people through direct contact. To prevent spreading them, practice good hygiene: wash your hands frequently, avoid sharing personal items, and keep any open wounds clean and covered.
When should I see a doctor for a suspected bacterial pustule?
It’s important to seek medical attention if you experience any of the following: signs of spreading infection (increased redness, swelling, fever), large, painful, or persistent pustules, pustules near the eyes, nose, or genitals, or signs of a MRSA infection.
What are the complications of untreated bacterial pustule infections?
Untreated bacterial pustules can lead to several complications, including the spread of infection to other areas of the body, the formation of larger abscesses or boils, cellulitis (a deeper skin infection), sepsis (a life-threatening blood infection), and scarring.
How to prevent bacterial pustules after a surgical procedure?
Following your doctor’s post-operative wound care instructions is crucial for preventing infections, including bacterial pustules. This typically involves keeping the wound clean and dry, changing bandages regularly, and monitoring for any signs of infection.
What is the difference between a boil and a bacterial pustule?
Both boils and bacterial pustules are skin infections, but boils are generally larger, more painful, and deeper than pustules. Boils often start as a red, tender bump and fill with pus over time, while pustules are typically smaller and more superficial.
What are effective over-the-counter treatments for small bacterial pustules?
Topical antibiotics, such as those containing bacitracin or neomycin, can be effective for treating small bacterial pustules. However, it’s important to use these products as directed and consult a doctor if the pustule doesn’t improve within a few days.
How long does it typically take for a bacterial pustule to heal?
Most minor bacterial pustules will heal within a week or two with proper home care. However, larger or more severe pustules may take longer to heal and may require medical treatment.
What are the signs of a serious bacterial pustule infection needing urgent care?
Signs of a serious bacterial pustule infection that require urgent care include: fever, chills, spreading redness or swelling, severe pain, pus drainage that is foul-smelling or bloody, and swollen lymph nodes.
How to distinguish between bacterial pustules and other skin conditions?
Distinguishing between bacterial pustules and other skin conditions can be tricky. Bacterial pustules are typically characterized by a pus-filled center, redness, and inflammation. Other skin conditions, such as acne, boils, blisters, and folliculitis, have different characteristics. If you’re unsure, it’s always best to consult a healthcare professional.
What are the risk factors for developing recurring bacterial pustules?
Several factors can increase the risk of developing recurring bacterial pustules, including a weakened immune system, poor hygiene, certain medical conditions (such as diabetes or eczema), and close contact with someone who has a bacterial skin infection.
What hygiene practices can help prevent the formation of bacterial pustules?
Key hygiene practices for preventing bacterial pustules include: washing your hands frequently with soap and water, keeping wounds clean and covered, avoiding sharing personal items, and showering regularly.
Are there any natural remedies to soothe the pain of bacterial pustules?
Warm compresses can help soothe the pain and discomfort associated with bacterial pustules. However, it’s important to remember that natural remedies do not treat the underlying bacterial infection. If you have a bacterial pustule, it’s essential to address the infection with proper hygiene, over-the-counter treatments, or medical care if necessary.
Conclusion
After delving into the details of bacterial pustules, I hope you feel more confident in your ability to recognize, manage, and prevent these common skin infections. Remember, bacterial pustules are small, pus-filled bumps on the skin caused by bacteria, most often Staphylococcus aureus (staph) or Streptococcus pyogenes (strep). They can appear anywhere on the body and are often uncomfortable and concerning.
Key takeaways to keep in mind:
- Bacterial pustules are caused by bacteria entering the skin through a break.
- They are characterized by a white or yellowish center filled with pus, surrounded by redness and inflammation.
- Most minor pustules can be treated with home care, such as warm compresses and gentle cleansing.
- It’s important to avoid picking or squeezing pustules, as this can worsen the infection and lead to scarring.
- Seek medical attention if you experience signs of spreading infection, large or painful pustules, pustules near sensitive areas, or signs of MRSA infection.
- Preventing bacterial pustules involves practicing good hygiene, keeping wounds clean and covered, and maintaining a healthy lifestyle.
By following these guidelines, you can effectively manage bacterial pustules and promote healthy skin. Remember, if you have any concerns, don’t hesitate to consult a healthcare professional for proper diagnosis and treatment.